AI is already helping African clinicians find disease earlier, route patients to the right care, and move lifesaving supplies faster. It learns from data and returns useful outputs that humans can act on, such as image reads, triage advice, and risk scores. The World Health Organization says the promise is real, but systems must be deployed with strong ethics, safety, and transparency.
The new front line of care
Across the continent, clinicians face the same constraints: few specialists, busy clinics, and long travel times for patients. Artificial intelligence can help by turning raw inputs into practical outputs. A chest X-ray becomes a probability that TB (tuberculosis) is present. A retinal photo becomes a simple “refer” or “reassure”. A short text exchange becomes a safe pathway to a nurse, a clinic, or self-care. Used well, AI widens the front door to care and speeds decisions. Used poorly, it can add noise or risk. The WHO’s guidance is clear: design and deploy with ethics and human rights at the core.
How AI helps today
Screening and diagnosis
Systems read medical images and highlight those most likely to be abnormal. In TB, computer-aided detection for chest X-rays helps focus confirmatory testing on the right people. In eye care, AI can spot signs of diabetic retinopathy from a fundus photo and prompt fast referral. In maternal health, AI-guided “sweeps” can help non-experts acquire basic ultrasound views. The theme is the same: speed the right patients to the right next step.
Triage and virtual front doors
AI chat and symptom-triage tools give patients a safe first stop. Rwanda has deployed digital triage services to complement clinician capacity. These systems can answer common questions, suggest next steps, and book care when needed.
Public health logistics
AI-assisted routing and autonomous drones shorten delivery times for blood and medicines in hard-to-reach areas. Results from Rwanda show faster deliveries and fewer expired blood products, which matters in maternal emergencies.
Case study 1: Rwanda’s AI eye screening (Esther’s story)
Diabetes is increasing, yet eye screening is scarce outside cities. Missing diabetic retinopathy (DR) leads to avoidable sight loss.
Esther, a woman living with diabetes in Rwanda, attended her first screening at a clinic using an AI retinal tool. The system analysed her images immediately, flagged significant DR in both eyes, and the clinic referred her to a partner hospital in Kigali for treatment. The point is simple: instant reads make same-day decisions possible, which reduces loss to follow-up.

A randomised trial in Rwanda found AI-supported DR screening improved referral uptake compared with standard pathways. Related implementation work reported high accuracy and very high patient satisfaction, with many patients valuing immediate results.
In clinics without ophthalmologists, AI turns a single visit into a decision point. Patients like Esther get to treatment faster and have a better chance of keeping their sight.
Case study 2: Nigeria’s mobile TB X-ray with AI triage
TB remains a leading killer. Many people with TB do not have obvious symptoms, and radiologists are scarce in rural areas.
Programmes in Nigeria partnered to deploy ultra-portable X-ray units with AI interpretation at community screening camps. People over 15 were screened. If symptoms or the AI score suggested TB, staff collected sputum for confirmatory testing. Studies from Nigeria show that this approach can improve active case-finding and offers a cost-effective screening path for remote populations.
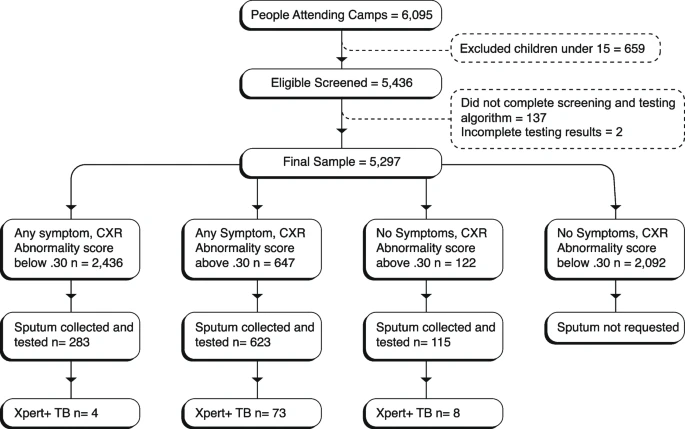
AI focuses scarce confirmatory tests on the highest-risk patients. Multi-country analyses show modern computer aided detection tools can achieve strong diagnostic accuracy, which helps teams find TB earlier while keeping workload under control.
How to make AI work in real clinics
- Target a clear gap: Pick use-cases where specialist capacity is thin and delays are costly: TB X-rays, DR screening, basic ultrasound, or triage.
- Keep clinicians in charge: AI flags; humans decide. Set thresholds, record reasons, and escalate uncertain cases. The WHO advises caution and clear accountability.
- Validate locally: Check performance on local populations and devices. Monitor accuracy, referral uptake, and patient outcomes over time.
- Design for real conditions. Plan for power cuts, spotty bandwidth, and staff rotations. Prefer tools that run at the edge or degrade gracefully.
- Explain decisions. Use simple messages that patients and staff understand, especially when systems suggest a referral or a block.
Risks and safeguards
- Bias and representativeness. Models trained elsewhere can underperform locally. Demand evidence from comparable settings and keep auditing.
- Privacy and consent. Health data is sensitive. Follow national data-protection laws and get consent right.
- Model drift. Populations and protocols change. Track performance and retrain.
- Over-reliance. AI can miss edge cases. Keep a human in the loop and design safe fallbacks.
- Governance. Align with the WHO’s ethics guidance and national rules to protect safety and trust.
Implementation playbook for providers
- Start with one journey. For example, add AI triage to a mobile TB X-ray van or introduce AI DR screening in diabetes clinics. Define success in advance: referral uptake, time to diagnosis, cost per positive case.
- Build the data path. Map data ownership, consent, and storage. Decide what runs on device and what runs in the cloud.
- Train the team. Short, role-specific sessions for nurses, radiographers, and community health workers.
- Close the loop. Feed confirmed outcomes back into the system. Track false positives and negatives.
- Report simply. Share results with staff and communities so trust grows with evidence, not hype.
Expect more validation studies on African datasets, especially for TB and maternal health. Look for national guidance on safe use of large language models in clinical workflows. Watch the expansion of drone-enabled supply chains that pair AI routing with automated delivery for emergency stock.
AI is not a silver bullet. It is a set of tools that, when matched to specific gaps and governed well, help African clinicians and patients move faster and decide better. Start small, measure what matters, keep people in the loop, and scale what works. That is how AI turns into healthier lives, not just clever software.
Get passive updates on African tech & startups
View and choose the stories to interact with on our WhatsApp Channel
ExploreLast updated: October 7, 2025